Intro
Sleep is important. No human, as reliant on their brain as a bird on its wings, can function without sufficient amount of it. The invisible god of sleep demands 7-9 hours each day to restore their thought- and memory powers [Davies 2022, Hoyos 2015, Lloyd-Jones 2022]. But there is more to good sleep than just duration. Its architecture is as if not even more important [Ohayon 2017].
If you are curious to know more about what makes quality sleep follow us into the exciting world of electroencephalography, brain activity and sleep patterns to learn about…
Sleep architecture
The sleep patterns
In humans, normal sleep consists of multiple phases that in the mental carousel of the night, unlike other mammals, take more abrupt turns than a Hummingbird on a sugar rush [McCarley 2007].
For the longest time, humans were only able to distinguish between different sleep phases by the movement of their eyes or lack thereof. Researches therefore chose the astoundingly fitting names of rapid eye movement sleep (REM sleep or REMS) and non rapid eye movement sleep (NREM sleep or NREMS) to distinguish between them.
Only later, when humanity tamed the powers of electricity and magnetism were they able to take a more distinguished look at the events of their sleeping brethren and found the following primary sleep-stages [Ohayon 2017]:
- NREM stage 1 sleep
- NREM stage 2 sleep
- NREM stage 3 sleep
- REM sleep
NREM stage 1 sleep
Stage 1 sleep is also known as sleep onset or relaxed wakefulness. Typically it takes about ≤5% of total sleep time in humans [Green 2017, Ohayon 2017].
If we were to borrow a scientists eyes and observe the world through them, this sleeping phase would appear indistinguishable from wakefulness. Humans woken up in this phase will typically not even realize that they have been asleep. It has therefore no impact on human health and should ideally take up as little time as possible [Houldin 2019].
NREM stage 2 sleep
NREMS is the second sleep stage that the brain loops in and out of. Under normal conditions it takes up more than 50% of the comfy duration [Ohayon 2017].
NREM stage 3 sleep
Stage 3 sleep is where it finally gets really interesting. The slow wave sleep (SWS), called like it for the rather slow EEG-waves, is the period to have for memory cleanup and consolidation; especially when it comes to declarative memory (intentionally remembering stuff) [Carlson 2012, Fowler 1973, Marshall 2006, Plihal 1997, Tucker 2006, Yaroush 1971].
It takes up only between 16%–20% of normal sleep [Ohayon 2017]. Until recently it was devided into stage 3 and stage 4 sleep.
REM sleep
And finally, there is rapid eye movement sleep, the party-girl of sleep. As the name implies, it is most widely known for its rather erratic movement of the pupils. It takes up to a third of a common human’s sleep 21%–30%, on a good night [Ohayon 2017].
While NREM sleep concentrates on the declarative side of things, REM sleep improves procedural (unconscious tasks), spatial (where is what; especially those darnish keys?) and emotional (remembering the true important things) memory [Born 2012, Rasch 2007, Wagner 2004, Zhang 2005, Zhang 2016].
By going hand in hand, REM and NREM sleep work together to consolidate the common human’s memory. Scientists even created a whole theory about it, called sequential hypothesis [Rasch 2013].
The order of sleep
Of course, the different sleep-phases don’t work simultaneously on the nightly repair-controls, but come one after the other.
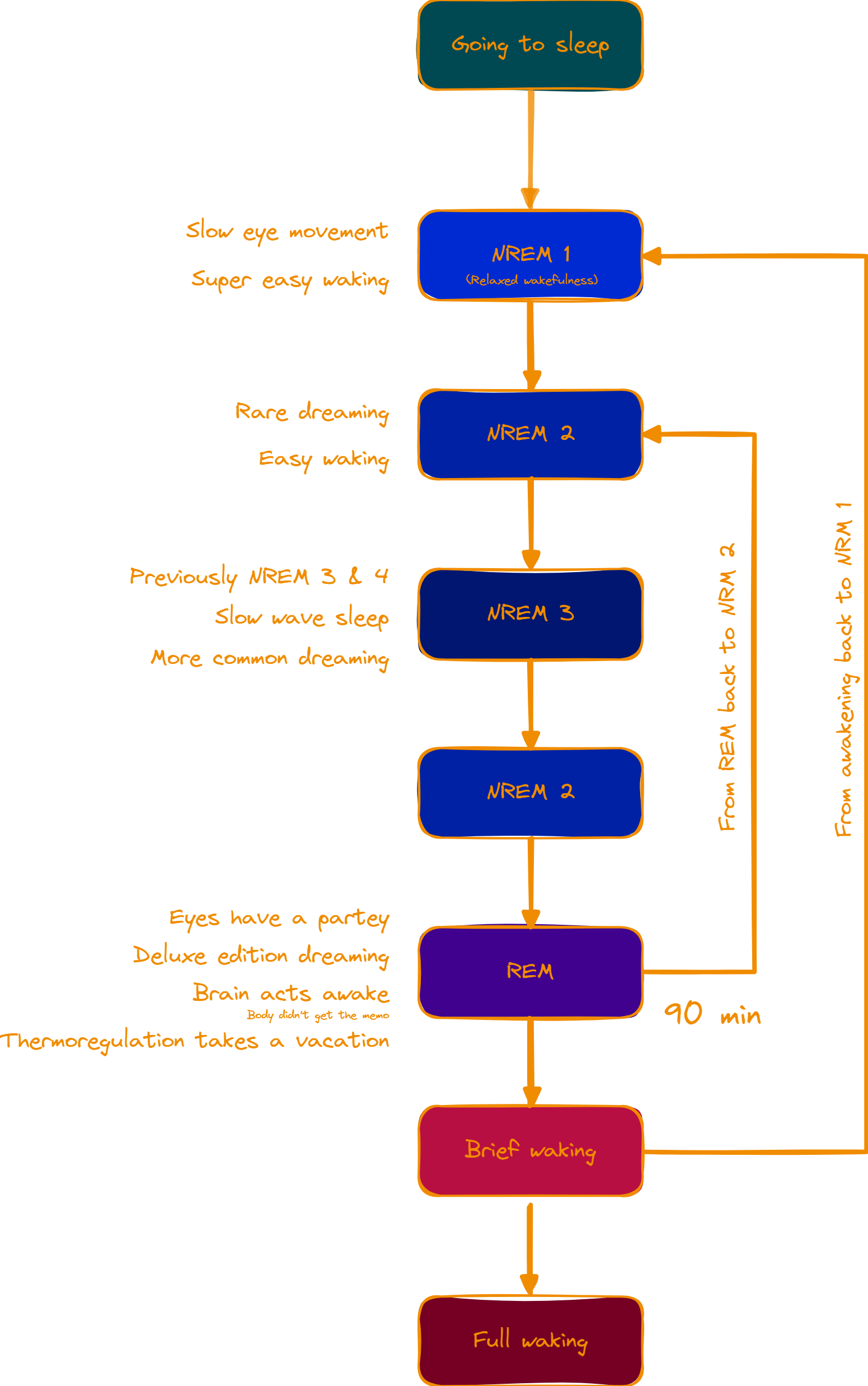
When a human lies to to rest, there is no sudden jump to deep sleep, but a gentle transition through the first phases. It typically starts with NREM stage 1 sleep and, despite its name, some eye movement [Green 2017].
At some point the sleep drive pushes all the necessary levers to transition the brain to stage 2. Some humans dream during this stage, but the grand stage of dreams lies ahead [Siclari 2017].
It begins with NREM stage 3, during which also the primary work for declarative memory consolidation and learning occurs [Peplow 2013]. During this stage, the brain replays previous experiences over and over again, as if it trapped the human in a time-loop, to move experiences to long-term memory [Born 2012, Rasch 2013]. Following a loop, the brain then returns to stage 2 sleep, before transitioning to REM.
From here the brain normally either returns to NREM2 or (briefly) awakens, which brings it back to NREM1. Either way, it repeats the cycle in 90 min intervals typically 4-5 times during a normal and healthy eight-hour sleep [Brancaccio 2020, Feinberg 1979, National Institutes of Health 2019, Peplow 2013, Peraita-Adrados 2005, Peter 2007, Rasch 2007, Silber 2007, Van Couter 2008].
Under atypical circumstances, that more often than not might make the norm, the pattern of sleep might look different. The human body will nevertheless always try to balance the sleep stages to meet the necessary quotas. This holds especially true for REM sleep.
If the brain registers insufficient amounts of REM sleep, it will go into a process scientists termed REM rebounding [Aeschbach 2011, Ellman 1991, Endo 1998]. With more vigor and greater focus than a cheated teenager it will grab the next REM stage available to make up for lost time (and show the ex-REM stage what’s up).

Outro
Sleep stages are the building blocks of a restful night. Their distribution and application is necessary for a healthy, open and focused mind.
Sources
| Key | Citation |
|---|---|
| Aeschbach 2011 | Aeschbach, D. (2011). REM-sleep regulation: circadian, homeostatic, and non-REM sleep-dependent determinants. Rapid Eye Movement Sleep: Regulation and Function. Cambridge University Press, Cambridge, 80-88. |
| Born 2012 | Born, J., & Wilhelm, I. (2012). System consolidation of memory during sleep. Psychological research, 76, 192-203. |
| Brancaccio 2020 | Brancaccio, A., Tabarelli, D., Bigica, M., & Baldauf, D. (2020). Cortical source localization of sleep-stage specific oscillatory activity. Scientific reports, 10(1), 6976. |
| Carlson 2012 | Carlson, N. R. (2012). Physiology of behavior. Pearson Higher Ed. |
| Davies 2022 | Davies, M. J., Aroda, V. R., Collins, B. S., Gabbay, R. A., Green, J., Maruthur, N. M., … & Buse, J. B. (2022). Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes care, 45(11), 2753-2786. |
| Ellman 1991 | Ellman, S. J., Spielman, A. J., Luck, D., Steiner, S. S., & Halperin, R. (1991). REM deprivation: A review. |
| Endo 1998 | Endo, T., Roth, C., Landolt, H. P., Werth, E., Aeschbach, D., Achermann, P., & Borbély, A. A. (1998). Selective REM sleep deprivation in humans: effects on sleep and sleep EEG. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 274(4), R1186-R1194. |
| Feinberg 1979 | Feinberg, I., & Floyd, T. C. (1979). Systematic trends across the night in human sleep cycles. Psychophysiology, 16(3), 283-291. |
| Fowler 1973 | Fowler, M. J., Sullivan, M. J., & Ekstrand, B. R. (1973). Sleep and memory. Science, 179(4070), 302-304. |
| Green 2017 | Green, S. (2017). Biological rhythms, sleep and hypnosis. Bloomsbury Publishing. |
| Houldin 2019 | Houldin, E. (2019). Resting state network dynamics across wakefulness and sleep (Doctoral dissertation, The University of Western Ontario (Canada)). |
| Hoyos 2015 | Hoyos, C., Glozier, N., & Marshall, N. S. (2015). Recent evidence on worldwide trends on sleep duration. Current Sleep Medicine Reports, 1, 195-204. |
| Lloyd-Jones 2022 | Lloyd-Jones, D. M., Allen, N. B., Anderson, C. A., Black, T., Brewer, L. C., Foraker, R. E., … & American Heart Association. (2022). Life’s essential 8: updating and enhancing the American Heart Association’s construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation, 146(5), e18-e43. |
| Marshall 2006 | Marshall, L., Helgadóttir, H., Mölle, M., & Born, J. (2006). Boosting slow oscillations during sleep potentiates memory. Nature, 444(7119), 610-613. |
| McCarley 2007 | McCarley, R. W. (2007). Neurobiology of REM and NREM sleep. Sleep medicine, 8(4), 302-330. |
| National Institutes of Health 2019 | National Institutes of Health. (2019). Brain Basics: Understanding Sleep. National Institute of Neurological Disorders and Stroke. |
| Ohayon 2017 | Ohayon, M., Wickwire, E. M., Hirshkowitz, M., Albert, S. M., Avidan, A., Daly, F. J., … & Vitiello, M. V. (2017). National Sleep Foundation’s sleep quality recommendations: first report. Sleep health, 3(1), 6-19. |
| Peplow 2013 | Peplow, Mark. (2013, May 22). Structure: The anatomy of sleep. Nature. https://www.nature.com/articles/497S2a#:~:text=In%20a%20typical%20eight-hour%20sleep%2C%20the%20brain%20moves,the%20brain%2C%20and%20is%20often%20associated%20with%20dreaming. |
| Peraita-Adrados 2005 | Peraita-Adrados, R. (2005). Electroencephalography, polysomnography, and other sleep recording systems. The physiologic nature of sleep, 103. |
| Peter 2007 | Peter, H., Penzel, T., & Peter, J. H. (Eds.). (2007). Enzyklopädie der Schlafmedizin. Berlin, Heidelberg: Springer Berlin Heidelberg. |
| Plihal 1997 | Plihal, W., & Born, J. (1997). Effects of early and late nocturnal sleep on declarative and procedural memory. Journal of cognitive neuroscience, 9(4), 534-547. |
| Rasch 2007 | Rasch, B., Büchel, C., Gais, S., & Born, J. (2007). Odor cues during slow-wave sleep prompt declarative memory consolidation. Science, 315(5817), 1426-1429. |
| Rasch 2013 | Rasch, B., & Born, J. (2013). About sleep’s role in memory. Physiological reviews. |
| Siclari 2017 | Siclari, F., Baird, B., Perogamvros, L., Bernardi, G., LaRocque, J. J., Riedner, B., … & Tononi, G. (2017). The neural correlates of dreaming. Nature neuroscience, 20(6), 872-878. |
| Silber 2007 | Silber, M. H., Ancoli-Israel, S., Bonnet, M. H., Chokroverty, S., Grigg-Damberger, M. M., Hirshkowitz, M., … & Iber, C. (2007). The visual scoring of sleep in adults. Journal of clinical sleep medicine, 3(02), 121-131. |
| Tucker 2006 | Tucker, M. A., Hirota, Y., Wamsley, E. J., Lau, H., Chaklader, A., & Fishbein, W. (2006). A daytime nap containing solely non-REM sleep enhances declarative but not procedural memory. Neurobiology of learning and memory, 86(2), 241-247. |
| Van Couter 2008 | Van Cauter, E., Spiegel, K., Tasali, E., & Leproult, R. (2008). Metabolic consequences of sleep and sleep loss. Sleep medicine, 9, S23-S28. |
| Wagner 2004 | Wagner, U., Gais, S., Haider, H., Verleger, R., & Born, J. (2004). Sleep inspires insight. Nature, 427(6972), 352-355. |
| Yaroush 1971 | Yaroush, R., Sullivan, M. J., & Ekstrand, B. R. (1971). Effect of sleep on memory: II. Differential effect of the first and second half of the night. Journal of experimental psychology, 88(3), 361. |
| Zhang 2005 | Zhang, J. (2005). Continual-activation theory of dreaming. Dynamical Psychology, 2005. |
| Zhang 2016 | Zhang, J. (2016). Towards a comprehensive model of human memory. |

Leave a Reply