After a strenuous day of work, the most remarkable things happens. As the night falls, the common human enters a special room set up for comfort and protection, lies down and closes their eyes. For hours, the homo sapiens remain like this, motionless in a state that might appear like death. The phenomenon called sleep takes up typically almost a third of a common human’s life [Killgore 2010]. But what might appear as a resting state could be far from it.
What happens when we sleep
Processes from macroscopic down to microscopic scale of their DNA are kicked off throughout the human. Their body temperature and heart rate fall. At the same time, ghrelin goes into overdrive and triggers the release of growth and regenerative hormones [Turek 1999, Dzaja 2004].
Sleep is therefore the primary regeneration period for humans [Cespuglio 2005]. But while these and other events could also happen during waking hours, this isn’t the case for the brain [Eugene 2015, Joiner 2016].
Sleep is of the brain, by the brain and for the brain.
[Hobson 2005]
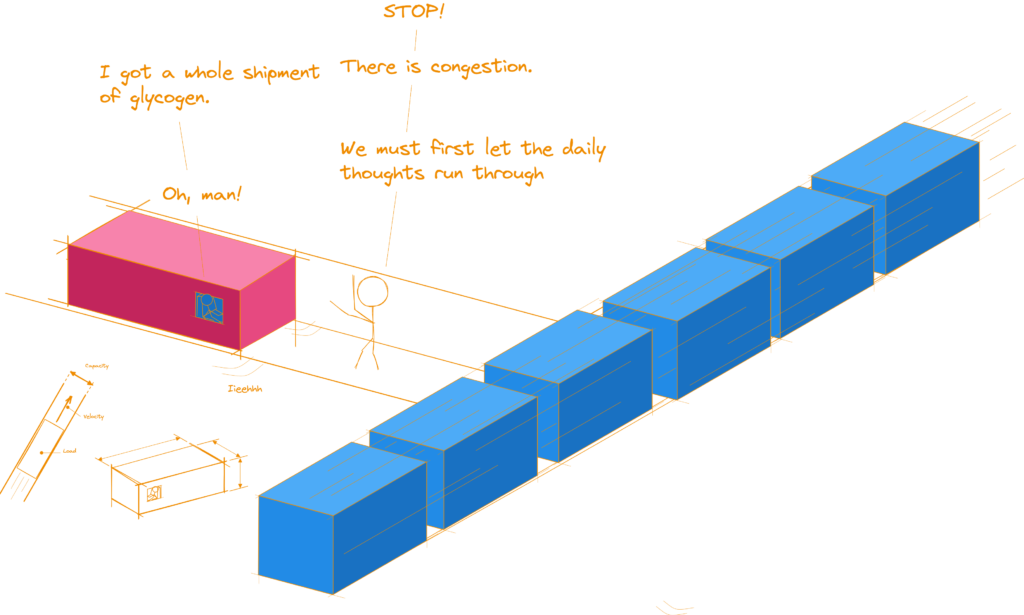
On one level, the human’s central control system powers down, severely reducing its energy consumption [Maquet 2005]. But that happens only to clear the paths for a cleanup that puts deep spring cleanings to shame. Waste products that accumulate during the neural processes of thinking (an ability humans especially pride themselves with) are decomposed and transported out the central nervous system. [Spiegel 2005]
At the same time, with the pathways clear, the brain recharges its glycogen-batteries in preparation of the next day [Cespuglio 2005].
Sleep and society
Most humans rarely think about these and all the numerous other processes that occur during sleep.
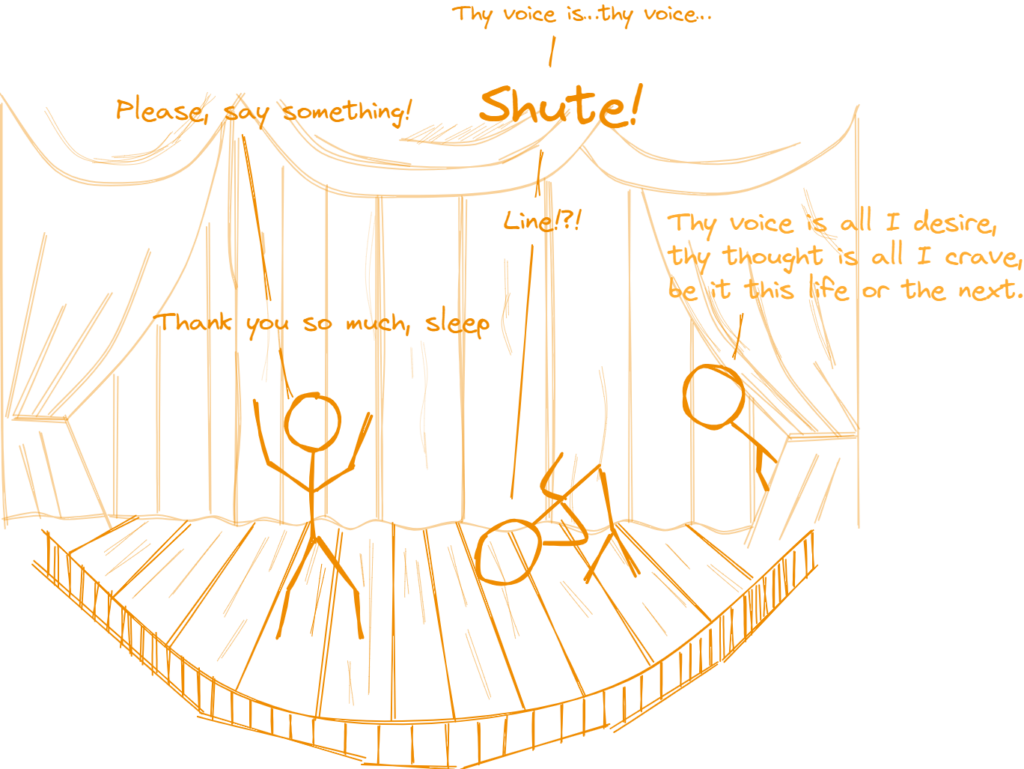
No one ever wrote a novel called “The pursuit of sleep” or lamented about its ups and downs in song and melody. The reason for it clear. Sleep isn’t a shining actor in humans’ lives. It isn’t happiness or love, the diva of life, or hunger.
It is more subtle, working behind the curtains instead of center stage. Sleep supports and holds up all other actors, may they be mental health, youth, general well being or happiness with the tedious stamina of Atlas. That is, as long as humans give it the necessary time. At least 7 hours per day sleep demands to do its magic [Hoyos 2015, Davies 2022, Lloyd-Jones 2022]
But these hours are too often regarded as a nuisance; a time-frame that has to be overcome. It might be for that very reason that humans make sleep one of their first victims when other obligations like work, school or their social life encroach. Whole professions, such as medical residents, military personnel and shift-workers, even go so far to put sleep on the sidelines and its deprivation in its place.
It is therefore no surprise that sleep loss is like an epidemic many humans don’t even realize they suffer from [Killgore 2010, Hoyos 2015, Ohayon 2017, Lloyd-Jones 2022, Rogers 2024].
And suffer they do.
What happens when humans don’t sleep (well) (enough)
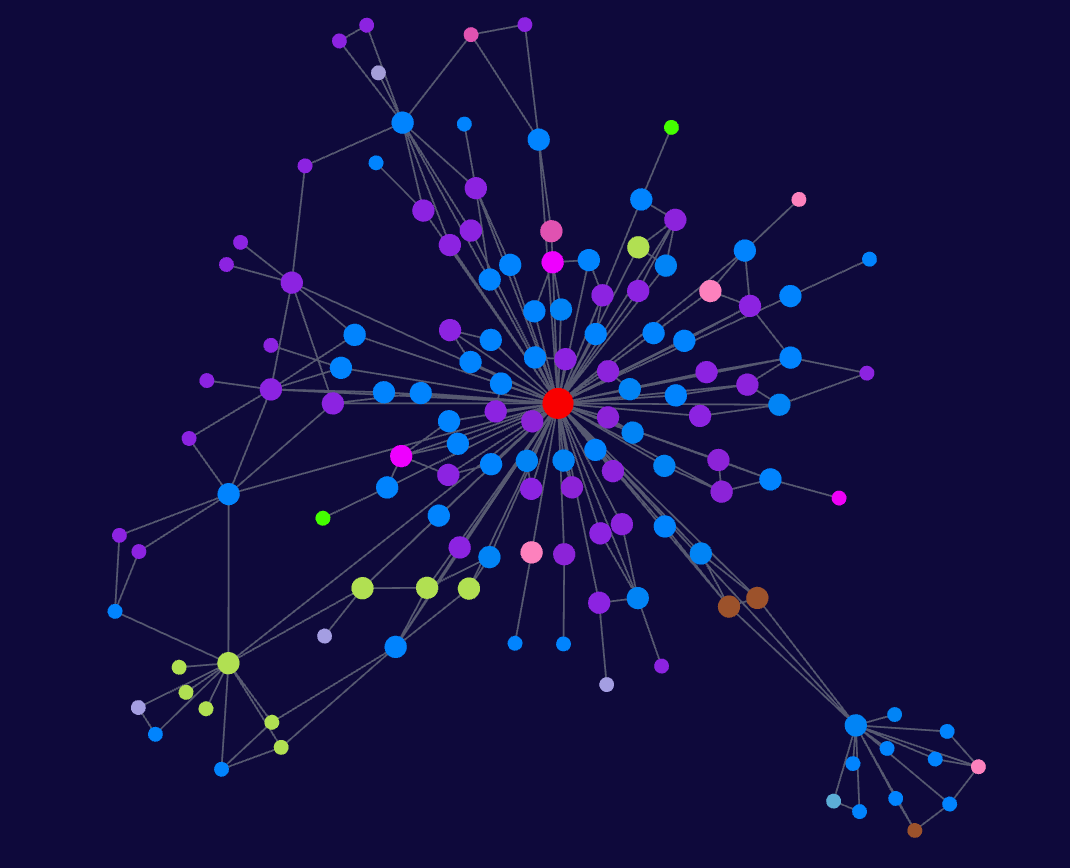
Sleep loss affects humans at every level of their being; be it their emotions, their ability to think, their perception, their health or the very bio-chemical processes within their individual cells [Andreazza 2010].
Mood
When humans sleep too little they turn into their worst selves. What is a shining face of smiles and compliments one day turns into a frown of blueness, irritation and frustration after as little as a single bad night. They react worse, become aggressive more easily and their social abilities melt away like ice under the sun [Chua 2006, Drummond 2006, Kahn-Greene 2006, Killgore 2008, Tempesta 2010, Killgore 2010].
Cognition
Cognition, one of, if not the most crucial quality the species of thinkers has carved their evolutionary niche out if, doesn’t fare much better under the weight of “not enough sleep” [Goel 2009].
Their creativity breaks down into a puddle of sorry excuses [Horne 1988, Harrison 2000-2].
When facing a decision a tired human will more often make the wrong choice [Killgore 2006-2, Lim 2008]. Not even the powers of caffeine are a remedy [Killgore 2007]. And as if that wasn’t enough, getting to that wrong choice also takes the sleep deprived human longer than in a wakeful state [Dongen 2003, Lim 2008, Goel 2009].
Probably worst is the hit memory and learning have to take. As it becomes harder and harder to focus, the sleep deprived human also has a more difficult time to pick up new information and store it in their long term memory [Drummond 2000, Walker 2006, Goel 2009, Walker 2009, Diekelmann 2010].
Senses
Also the senses take a hit.
The typical human relies heavily on their visual perception. Therefore it is a shame that in a sleep deprived state colors lose intensity and the field of vision shrinks [Roge 2009.]
Hearing too is impacted, as is smelling, tasting and even touch. The pain threshold declines, making a tired human more susceptible to injuries [Furchtgott 1956, Kundermann 2004, Babkoff 2005, Killgore 2006, Haack 2009].
Disease
Then there is disease. At it turns out, sleep is a king when it comes to keeping humans healthy [Majde 2005]. Obesity, insulin resistance, type 2 diabetes and worse degradation of the brain are all ailments sleep deprivation can cause in humans [Harrison 2000, Harrison 2000-2, Jones 2001, Spiegel 2005, Knutson 2008, Donga 2010].

Outro
Sleep is a core of life, and although the effects differ from human to human, the underlying detriment to health, happiness and productivity remain when they are deprived from it [Killgore 2010].
All humans are created equal but some humans are created more equal
It is therefore save to say, don’t see sleep as a waste of time, but a necessary step to keep you running.
Sources
| Key | Citation |
|---|---|
| Andreazza 2010 | Andreazza, A. C., Andersen, M. L., Alvarenga, T. A., de-Oliveira, M. R., Armani, F., Ruiz, F. S., … & Tufik, S. (2010). Impairment of the mitochondrial electron transport chain due to sleep deprivation in mice. Journal of psychiatric research, 44(12), 775-780. |
| Babkoff 2005 | Babkoff, H., Zukerman, G. I. L., Fostick, L., & Ben‐Artzi, E. L. I. S. H. E. V. A. (2005). Effect of the diurnal rhythm and 24 h of sleep deprivation on dichotic temporal order judgment. Journal of sleep research, 14(1), 7-15. |
| Cespuglio 2005 | Cespuglio, R., Colas, D., & Gautier-Sauvigné, S. (2005). Energy processes underlying the sleep–wake cycle. In The Physiologic Nature of Sleep (pp. 3-21). |
| Chua 2006 | Chuah, Y. L., Venkatraman, V., Dinges, D. F., & Chee, M. W. (2006). The neural basis of interindividual variability in inhibitory efficiency after sleep deprivation. Journal of Neuroscience, 26(27), 7156-7162. |
| Davies 2022 | Davies, M. J., Aroda, V. R., Collins, B. S., Gabbay, R. A., Green, J., Maruthur, N. M., … & Buse, J. B. (2022). Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes care, 45(11), 2753-2786. |
| Diekelmann 2010 | Diekelmann, S., & Born, J. (2010). The memory function of sleep. Nature reviews neuroscience, 11(2), 114-126. |
| Donga 2010 | Donga, E., van Dijk, M., van Dijk, J. G., Biermasz, N. R., Lammers, G. J., van Kralingen, K. W., … & Romijn, J. A. (2010). A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. The Journal of Clinical Endocrinology & Metabolism, 95(6), 2963-2968. |
| Dongen 2003 | Van Dongen, H. P., Maislin, G., Mullington, J. M., & Dinges, D. F. (2003). The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep, 26(2), 117-126. |
| Drummond 2000 | Drummond, S. P., Brown, G. G., Gillin, J. C., Stricker, J. L., Wong, E. C., & Buxton, R. B. (2000). Altered brain response to verbal learning following sleep deprivation. Nature, 403(6770), 655-657. |
| Drummond 2006 | Drummond, S. P., Paulus, M. P., & Tapert, S. F. (2006). Effects of two nights sleep deprivation and two nights recovery sleep on response inhibition. Journal of sleep research, 15(3), 261-265. |
| Dzaja 2004 | Dzaja, A., Dalal, M. A., Himmerich, H., Uhr, M., Pollmächer, T., & Schuld, A. (2004). Sleep enhances nocturnal plasma ghrelin levels in healthy subjects. American Journal of Physiology-Endocrinology and Metabolism, 286(6), E963-E967. |
| Eugene 2015 | Eugene, A. R., & Masiak, J. (2015). The neuroprotective aspects of sleep. MEDtube science, 3(1), 35. |
| Furchtgott 1956 | Furchtgott, E., & Willingham, W. W. (1956). The effect of sleep-deprivation upon the thresholds of taste. The American Journal of Psychology. |
| Goel 2009 | Goel, N., Rao, H., Durmer, J. S., & Dinges, D. F. (2009, September). Neurocognitive consequences of sleep deprivation. In Seminars in neurology (Vol. 29, No. 04, pp. 320-339). © Thieme Medical Publishers. |
| Haack 2009 | Haack, M., Lee, E., Cohen, D. A., & Mullington, J. M. (2009). Activation of the prostaglandin system in response to sleep loss in healthy humans: potential mediator of increased spontaneous pain. Pain, 145(1), 136-141. |
| Harrison 2000 | Harrison, Y., Horne, J. A., & Rothwell, A. (2000). Prefrontal neuropsychological effects of sleep deprivation in young adults–a model for healthy aging?. Sleep, 23(8), 1067-1073. |
| Harrison 2000-2 | Harrison, Y., & Horne, J. A. (2000). The impact of sleep deprivation on decision making: a review. Journal of experimental psychology: Applied, 6(3), 236. |
| Hobson 2005 | Hobson, J. A. (2005). Sleep is of the brain, by the brain and for the brain. Nature, 437(7063), 1254-1256. |
| Horne 1988 | Horne, J. A. (1988). Sleep loss and “divergent” thinking ability. Sleep, 11(6), 528-536. |
| Hoyos 2015 | Hoyos, C., Glozier, N., & Marshall, N. S. (2015). Recent evidence on worldwide trends on sleep duration. Current Sleep Medicine Reports, 1, 195-204. |
| Joiner 2016 | Joiner, W. J. (2016). Unraveling the evolutionary determinants of sleep. Current biology, 26(20), R1073-R1087. |
| Jones 2001 | Jones, K., & Harrison, Y. (2001). Frontal lobe function, sleep loss and fragmented sleep. Sleep medicine reviews, 5(6), 463-475. |
| Kahn-Greene 2006 | Kahn-Greene, E. T., Lipizzi, E. L., Conrad, A. K., Kamimori, G. H., & Killgore, W. D. (2006). Sleep deprivation adversely affects interpersonal responses to frustration. Personality and Individual Differences, 41(8), 1433-1443. |
| Killgore 2006 | Killgore, W. D., & McBride, S. A. (2006). Odor identification accuracy declines following 24 h of sleep deprivation. Journal of sleep research, 15(2), 111-116. |
| Killgore 2006-2 | Killgore, W. D., Balkin, T. J., & Wesensten, N. J. (2006). Impaired decision making following 49 h of sleep deprivation. Journal of sleep research, 15(1), 7-13. |
| Killgore 2007 | Killgore, W. D., Lipizzi, E. L., Kamimori, G. H., & Balkin, T. J. (2007). Caffeine effects on risky decision making after 75 hours of sleep deprivation. Aviation, space, and environmental medicine, 78(10), 957-962. |
| Killgore 2008 | Killgore, W. D., Kahn-Greene, E. T., Lipizzi, E. L., Newman, R. A., Kamimori, G. H., & Balkin, T. J. (2008). Sleep deprivation reduces perceived emotional intelligence and constructive thinking skills. Sleep medicine, 9(5), 517-526. |
| Killgore 2010 | Killgore, W. D. (2010). Effects of sleep deprivation on cognition. Progress in brain research, 185, 105-129. |
| Knutson 2008 | Knutson, K. L., & Van Cauter, E. (2008). Associations between sleep loss and increased risk of obesity and diabetes. Annals of the New York Academy of Sciences, 1129(1), 287-304. |
| Kundermann 2004 | Kundermann, B., Spernal, J., Huber, M. T., Krieg, J. C., & Lautenbacher, S. (2004). Sleep deprivation affects thermal pain thresholds but not somatosensory thresholds in healthy volunteers. Psychosomatic medicine, 66(6), 932-937. |
| Lim 2008 | Lim, J., & Dinges, D. F. (2008). Sleep deprivation and vigilant attention. Annals of the new York Academy of Sciences, 1129(1), 305-322. |
| Lloyd-Jones 2022 | Lloyd-Jones, D. M., Allen, N. B., Anderson, C. A., Black, T., Brewer, L. C., Foraker, R. E., … & American Heart Association. (2022). Life’s essential 8: updating and enhancing the American Heart Association’s construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation, 146(5), e18-e43. |
| Majde 2005 | Majde, J. A., & Krueger, J. M. (2005). Links between the innate immune system and sleep. Journal of Allergy and Clinical Immunology, 116(6), 1188-1198. |
| Maquet 2005 | Maquet, P. A., Sterpenich, V., Albouy, G., Dang-Vu, T., Desseilles, M., Boly, M., … & Peigneux, P. (2005). Brain imaging on passing to sleep. In The Physiologic Nature of Sleep (pp. 123-137). |
| Ohayon 2017 | Ohayon, M., Wickwire, E. M., Hirshkowitz, M., Albert, S. M., Avidan, A., Daly, F. J., … & Vitiello, M. V. (2017). National Sleep Foundation’s sleep quality recommendations: first report. Sleep health, 3(1), 6-19. |
| Roge 2009 | Rogé, J., & Gabaude, C. (2009). Deterioration of the useful visual field with age and sleep deprivation: insight from signal detection theory. Perceptual and motor skills, 109(1), 270-284. |
| Rogers 2024 | Rogers, E. M., Banks, N. F., & Jenkins, N. D. (2024). The effects of sleep disruption on metabolism, hunger, and satiety, and the influence of psychosocial stress and exercise: A narrative review. Diabetes/metabolism research and reviews, 40(2), e3667. |
| Spiegel 2005 | Spiegel, K., Knutson, K., Leproult, R., Tasali, E., & Van Cauter, E. (2005). Sleep loss: a novel risk factor for insulin resistance and Type 2 diabetes. Journal of applied physiology. |
| Tempesta 2010 | Daniela, T., Alessandro, C., Giuseppe, C., Fabio, M., Cristina, M., & Michele, F. (2010). Lack of sleep affects the evaluation of emotional stimuli. Brain research bulletin, 82(1-2), 104-108. |
| Turek 1999 | Turek, F. (1999). Circadian and Sleep Control of Hormonal Secretions. In Regulation of Sleep and Circadian Rhythms (pp. 423-452). CRC Press. |
| Walker 2006 | Walker, M. P., & Stickgold, R. (2006). Sleep, memory, and plasticity. Annu. Rev. Psychol., 57, 139-166. |
| Walker 2009 | Walker, M. P., & van Der Helm, E. (2009). Overnight therapy? The role of sleep in emotional brain processing. Psychological bulletin, 135(5), 731. |

Leave a Reply